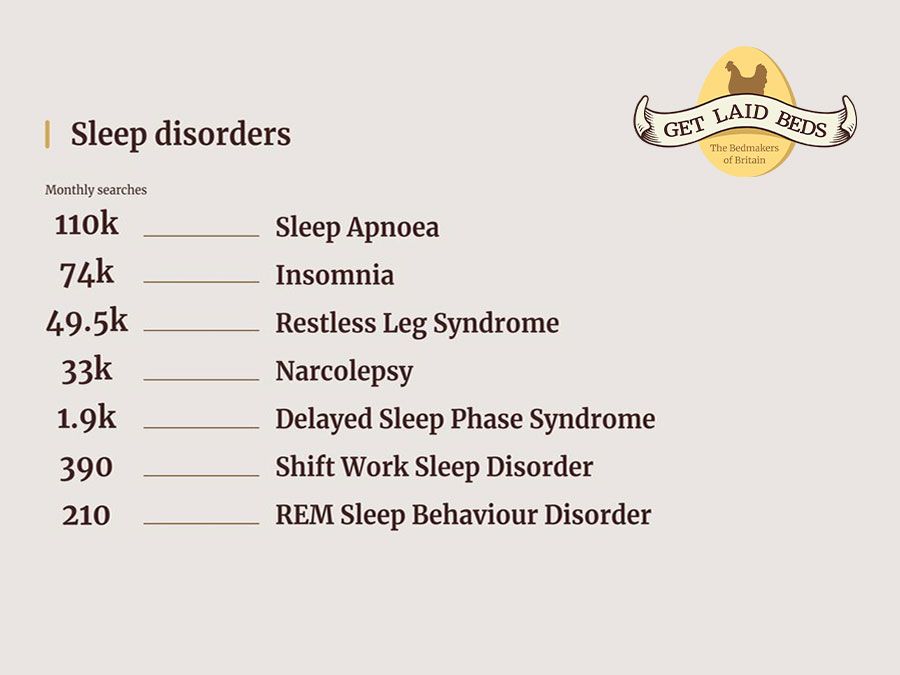
Sleep disorders affect around 20%, or 1 in 5, of the UK’s population. Getting enough high-quality sleep is imperative for good physical and mental health, so if you’re not sleeping well, it could be time to take action.
Many people with sleep disorders are unaware they have them. Have you noticed a pattern of disturbed sleep? Perhaps you find it difficult to fall asleep in the first place? These could be a symptom of a wider issue.
Below, Dr. Daisy Mae explains some of the most common sleep disorders, how to get better sleep, and when it’s time to book a visit to your GP.
Sleep Apnoea is a common condition affecting 1 in 8 UK adults, most of whom are unaware they have it. It occurs due to loss of muscle tone in the back of the throat and upper airways.
Symptoms of sleep apnoea include daytime sleepiness, which can result in falling asleep while driving or watching TV, headaches, bad temper and irritability, anxiety, depression, and loss of libido. Untreated, sleep apnoea increases the risk of heart attacks, strokes, type-2 diabetes and could even reduce your lifespan.
The good news is that sleep apnoea can be successfully treated. Simple measures such as stopping smoking, losing weight, and treating acid reflux can help. See your GP for an accurate diagnosis.
The most effective treatments are the use of a mandibular device, a specialised mouthpiece which pulls the jaw forward and holds the airway open at night, or the use of continuous positive airways pressure (CPAP).

36% of UK adults have insomnia, which is the extreme difficulty of falling asleep at least once a week or waking frequently at night.
Chronic insomnia takes its toll on health, increasing the risk of high blood pressure, heart disease and strokes, and reducing life span. Less than 7 hours of sleep per night increase the risk of death by 12% compared to those who get the required amount of sleep. Insomnia causes stress and exacerbates depression and anxiety, which can manifest itself in day-to-day difficulties, such as poorer work performance and a higher risk of road traffic accidents.
Fortunately, much can be done to help insomnia. Start with improving sleep hygiene, and take the following steps:
· Ensure you are sleeping in a cool, dark bedroom, in a comfortable bed - you should change your mattress every 7 years.
· Use hypoallergenic, clean bedding to avoid irritation in the night from allergens.
· Adopt a regular sleep routine, going to bed at the same time every night and waking at the same time every morning.
· When you wake up, open the curtains and flood the room with natural light.
· Wind down for sleep with soft music and a gentle bedtime routine, like engaging in reading or yoga.
· Do not use blue light devices within 2 hours of bedtime as this inhibits the production of the sleep hormone, melatonin.
· Avoid caffeine and alcohol for 6 hours before bedtime.
If, despite this, things are not improving, see your GP. You may need counselling or treatment for stress, anxiety, or depression. Cognitive behavioural therapy (CBT) can be very helpful. Note that sleeping tablets are not usually the answer.
Restless leg syndrome (RLS), also called Willis Ekbom disease, is a strange condition in which sufferers have an irresistible urge to move their legs at night, and often complain of sensations in their legs such as pricking or crawling. The condition affects 5-10% of adults, including during pregnancy, and it can also occur in children. A lot is still unknown about restless leg syndrome, including what causes it, although it may have a genetic component.
Treating RLS is difficult. It's important to avoid alcohol, caffeine, and smoking as these are known to worsen symptoms. Good sleep hygiene and participating in regular physical exercise are both very important.
In one study, those who followed a regular fitness regime for 6 weeks reported a 39% improvement in their RLS symptoms, as compared to an 8% improvement in the group who took no exercise. Compressing the legs with compression socks has also been found to give some relief, as well as hot and cold therapy and massage.
DSPS affects around 15% of the population, most of whom are young adults. In this condition, sleep is delayed for around 2 hours after going to bed. For example, those who go to bed at 10pm do not fall asleep until midnight. It is thought to be a Circadian rhythm disorder - note that this is different from being a night owl, as night owls are choosing to stay awake and go to bed later.
Because they fall asleep so late, DSPS sufferers have trouble waking up on time for work or school and experience excessive daytime sleepiness.
Those with DSPS are advised to go to bed 2 hours later than their usual bedtime every 5 or 6 days. They should also use a light box as soon as they wake up for 30 minutes a day as it switches off melatonin production and helps reset the Circadian body clock.

Shift work sleep disorder is a common condition affecting those who do shift work. They often come home after a night shift and try to sleep during the day, but the sleep cues are all wrong. Daylight switches off melatonin production, so the body's natural Circadian rhythms program the body to sleep at night, not during the day. As a result, the person cannot sleep when they need to sleep and suffers from insomnia, daytime sleepiness, and fatigue.
This condition is hard to treat, but you can try the following for the best possible results:
· Try not to do more than 5 night shifts in a row, and take at least 48 hours off after this before starting again.
· Avoid sunlight on the way home in the morning – wear sunglasses on the journey.
· Have a nap before a night shift.
· Avoid caffeine on the night shift within 6 hours of needing to go home and getting into bed.
· Take care if you need to drive home, as sleep deprivation is known to make people drowsy at the wheel and increases the risk of road accidents.
Your GP may prescribe melatonin if you’re struggling to sleep due to your shift pattern.

REM Sleep Behaviour Disorder occurs when a person is having REM sleep, but instead of their muscles being paralysed, as usually happens, their muscles remain active, and they act out their dreams. They can be very restless, kicking, punching, and even crying out – in fact, 60% of spouses of people with REM Sleep Behaviour Disorder have been injured by their partner during sleep.
The exact cause of this condition is not known. It often occurs in those who are later diagnosed with a major neurological condition such as Parkinson’s Disease or Lewy Body dementia.
The treatment of choice is melatonin, but this needs to be prescribed by a sleep physician to get the correct dose. Alternatively, an effective option is clonazepam, but this is more likely to cause side effects such as daytime somnolence and can increase the risk of falls.
As soon as someone starts showing signs of REM Sleep Behaviour Disorder, their bedroom needs to be modified to ensure there is no clutter, sharp objects, wires, or anything that could cause a night-time injury.

Narcolepsy is a much rarer medical condition, affecting 1 in 2-3,000 people. The cause is not well understood, but the brains of those with narcolepsy contain lower levels of a chemical called hypocretin, which is involved in the regulation of sleep and wakefulness.
There are five classic signs of narcolepsy:
· Excessive daytime sleepiness.
· Cataplexy (a sudden weakness that can cause collapse).
· Sleep paralysis (being unable to move when falling asleep or waking up).
· Hypnagogic hallucinations (frightening, vivid dreams).
· Insomnia.
Treating narcolepsy, much like with the other sleep disorders listed so far, involves attention to sleep hygiene, and reducing triggers such as alcohol, caffeine, and smoking. Take regular exercise and avoid taking any sedatives. Medication may be given such as dexamphetamine, methylphenidate, or antidepressants, but narcolepsy needs to be diagnosed and managed by a sleep physician.
If your sleep issues have lasted 3 months and are not improving, it’s time to seek help. Not getting enough sleep is dangerous for your physical and mental health and can even shorten your life expectancy. Once a diagnosis has been made, there is much that can be done to help, for example, you may be referred to a specialist sleep physician and require specialised tests such as an electroencephalogram (EEG) and/or polysomnography (sleep study).
Don’t let bad sleep damage your health – see your GP if sleep problems are persistent and getting you down, sooner rather than later.
Sleep disorders are not something to be taken lightly. However, an uncomfortable bed frame certainly won’t help your scenario.
At Get Laid Beds, all our handmade wooden bed frames are bespoke. You know you’re in good hands as we’ll design your bedframe just for you, available in 17 different colour and hardwood finishes, as well as tonnes of different designs and sizes. We’ll help you construct the most comfortable bed possible, complete with mattress and bedding.
Get in touch to find out more and start designing the wooden bed of your dreams for a better night’s sleep.


WE VALUE YOUR PRIVACY
We use cookies to enhance your browsing experience, serve personalised ads or content, and analyse the traffic with 3rd party services. By clicking ‘Accept’, you consent to our use of cookies, visit our Privacy Policy and our Cookie Policy for more info.
Please select one of the delivery countries below or navigate to our UK website for UK delivery options.
Note: International shipping prices are charged per bed rather than per order. This is due to the bulky nature and weight of these products.